Influenza: A Complex Troublemaker
By Amanda Riley
Ah, November—the smell of pumpkin spice, the crisp fall weather, the quickly approaching holidays; what’s not to like? Except of course the sound of coughing and sneezing to remind you that this time of year means flu season.
There are three main types of flu: A, B and C [1]. You’ve probably mostly heard about A viruses, which are classified as either H1N1 (“swine” flu) or H3N2, and strains are identified based on where and when the virus is isolated [1]. New strains are created when a virus changes its outer appearance (more on this later!) and genetic material [2]. H1N1 gained a lot of attention because of the 2009 outbreak; CDC scientists believe that the strain involved came about when a virus in North American pigs and a virus in Eurasian pigs mixed their genetic material [3]. A virus such as this had never been seen before, and its ability to infect humans led many to become sick with influenza [3]. Since viruses can constantly exchange genes to create new strains, it is extremely difficult to control the flu, and we cannot use the same vaccine every year. The World Health Organization (WHO) predicts which strains are going to be most prevalent for the upcoming season; however, these predictions are difficult to make due to the complexity of the virus [4].
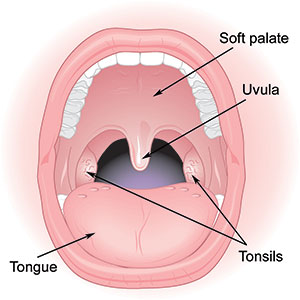
Research from early October of this year provides more insight on the complicated nature of H1N1 [5]. Scientists found that the virus may preferentially infect the soft palate [5]; what does that mean exactly? First off, the soft palate refers to the area of the mouth shown in Image 1. Prior to these discoveries, the soft palate wasn’t heavily researched in influenza studies (the focus tended to be on the lungs and nose) [5]. When the researchers say the virus preferentially infects the soft palate, they are referring to the ability of the virus to invade a healthy region of the body and cause trouble. The soft palate is composed of spherical cells that are similar in shape to the virus shown in Image 2, but cells are much larger than viruses. Infection begins when the virus gets inside one of these cells, but first it has to attach itself to the outside of the cell (known as the cell surface) [5]. It’s easier to handle an object when you have a firm grip on it as opposed to trying to hold it with a few fingers; similarly, the virus must be anchored to the cell before it can gain entry [5].
Attachment of the virus to the host cell is facilitated by receptors, which are little structures that jut out from viruses and cell surfaces. On the flu virus, these receptors are called Hemagglutinins, and they attach to cell surface receptors known as glycans (see Image 2) [5]. Just as there are numerous strains of flu, there are several types of Hemagglutinin; also, cells have different glycans depending on where that cell is located in the body [5]. This attachment is specific, meaning that Hemagglutinin “X” can bind to glycan “X” but not glycan “Y” [5].
After binding to and entering the soft palate cell, the flu provokes the cell to release chemicals that increase blood flow to the soft palate, resulting in swelling [6]. The soft palate has sensors that can stimulate sneezing, and swelling over-activates these sensors such that someone sneezes more than usual [5]. This is problematic because the flu virus can travel through the air in saliva and mucus, so sneezing causes someone to transfer the virus to someone else [5]. The soft palate could be essential for learning more about how the virus spreads from person to person because this region of the mouth is likely one of the first areas the virus encounters [5]. Although this study was conducted in ferrets, human soft palate cells have the same glycans as ferret soft palate cells [5], so these results are relevant to understanding and preventing influenza infection in humans.
Thanks to scientists around the world, thousands of lives can be saved with the seasonal flu vaccine. From 2010-2012, vaccinated children (6 months to 17 years old) were 74% less likely to be hospitalized from the flu compared to unvaccinated children [7]. Since the vaccine changes every season, pharmaceutical companies have to work around the clock to develop a safe, effective vaccine before too many people get sick. It is not uncommon for companies to devote whole facilities to flu vaccine. If pharmaceutical companies did not produce a flu vaccine, it’s scary to think about what might happen each flu season. Massive, global outbreaks? Millions of people infected? Yet even in the face of these potential consequences, many people are hesitant to get vaccinated. The root of this skepticism appears to be a general mistrust in the WHO and “Big Pharma” companies who are often seen as greedy and corrupted [4]. However, these preconceived notions undermine the admirable work required to produce the annual vaccine.
The soft palate study illustrates that we are still in the process of learning about the virus; nevertheless, scientists have done an incredible job of preventing millions of illnesses and deaths! Even though we don’t know all the details about the many strains of influenza, this doesn’t mean that the vaccine is useless or completely inefficient. As our knowledge of the virus increases, so too will the efficacy of the vaccine; will we ever be able to create a perfect vaccine? It’s hard to say; viruses are incredibly complicated, but pharmaceutical companies—aided and informed by scientists around the world—have made commendable progress in understanding the flu and developing an annual vaccine to prevent infections. Because of this, we should take advantage of the protection granted by the vaccine (get your flu shot!) and appreciate, rather than criticize, the intense dedication and research that goes into understanding this complex virus.
References
1. Types of Influenza Viruses Centers for Disease Control and Prevention [updated 19 August 2014]. Available from: http://www.cdc.gov/flu/about/viruses/types.htm.
2.How the Flu Virus Can Change: "Drift" and "Shift": The Centers for Disease Control and Prevention [updated 19 August 2014]. Available from: http://www.cdc.gov/flu/about/viruses/change.htm.
3. Origin of 2009 H1N1 (Swine Flu): Questions and Answers The Centers for Disease Control and Prevention [updated 25 November 2009]. Available from: http://www.cdc.gov/h1n1flu/information_h1n1_virus_qa.htm - a.
4. Abeysinghe S. Vaccine Narratives and Public Health: Investigating Criticisms of H1N1 Pandemic Vaccination. PLoS Curr. 2015;7.
5. Lakdawala SS, Jayaraman A, Halpin RA, Lamirande EW, Shih AR, Stockwell TB, et al. The soft palate is an important site of adaptation for transmissible influenza viruses. Nature. 2015;526(7571):122-5.
6. Julkunen I, Melen K, Nyqvist M, Pirhonen J, Sareneva T, Matikainen S. Inflammatory responses in influenza A virus infection. Vaccine. 2001;19:S32-S7.
7. Ferdinands JM, Olsho LE, Agan AA, Bhat N, Sullivan RM, Hall M, et al. Effectiveness of influenza vaccine against life-threatening RT-PCR-confirmed influenza illness in US children, 2010-2012. J Infect Dis. 2014;210(5):674-83.
Amanda Riley ('16) is a senior Biology major at Muhlenberg College with minors in French and Public Health.
After college, she's interested in pursuing a career as a research scientist but is hoping to gain more work experience before going to graduate school. She's had internships within the pharmaceutical industry and also within academia, but she would like to continue learning about fields of biomedical research.
Working with influenza vaccine during a previous internship was a challenging but rewarding experience that made her think about pursuing vaccine development.
Wherever her career takes her, she hopes to have the opportunity to travel. She studied abroad in Geneva, Switzerland during the Spring 2015 semester and had an incredible time! She took public health and french classes, lived with a french-speaking homestay family, visited international organizations (including the World Health Organization!) and traveled with friends.
She would love to return to Europe someday, maybe working as a research scientist!
Amanda's LinkedIn Profile